Introduction
The word LASER is an acronym for "light amplification by stimulated emission of radiation”. Lasers generate light energy in the form of a beam of photons released from the medium contained in the laser device. This generally gives the laser its name (CO2, erbium) and defines its specific wavelength. Current medical lasers emit wavelengths from the ultraviolet to the mid-infrared spectrum. The medium is activated with some form of energy, which is usually light or electricity. The stimulated emission of photons occurs in the medium and the light is then amplified in the laser cavity by mirrors, to be emitted from the front mirror as a single beam of light energy. The photons are identical and precisely synchronized in the temporal and spatial phases, and are all a single colour (monochromatic). The beam is more or less parallel; this characteristic is called collimation. The sum of these three components is coherence. This coherence is what gives a laser beam its exceptionally high photonic intensity and allows a laser ray to focus on very small points.
The main biological targets of lasers are blood (haemoglobin), melanin and water. These absorb the energy of light very differently and have optimal absorption spectra depending on the wavelength of the incident photon energy. Laser treatment has been used safely and effectively in many areas, such as dermatology, dentistry, ophthalmology and aesthetic medicine. In recent years, several innovative publications on the use of lasers in gynaecology have emerged, mirroring the benefits observed in other medical specialities.
The three physical characteristics that have made it possible to use lasers in the vulvovaginal areas are: their minimal micron ablation, or even non-ablation, along with their thermal effects; their absorption coefficient, which in this case corresponds to the water of the vagina (90% of the vagina is water); and finally the fact that they are fractional, which means that the surrounding healthy tissue recovers and regenerates the tissue affected by laser action quickly and without discomfort [1].
In gynaecology, the three basic indications where lasers have been shown to be effective are: vulvovaginal atrophy (VVA)/genitourinary syndrome of menopause (GSM), vaginal hyperlaxity syndrome, and stress urinary incontinence (SUI) [2]. There are also studies in other diseases such as genital prolapse and vulvar lichen, but more evidence is needed.
The possible mechanisms by which laser treatment may improve SUI are its biostimulant and photothermal effects. Laser biostimulation restores most vaginal functions, including secretion, absorption, elasticity, lubrication and thickness of the vaginal epithelium [3], while the photothermal effect produced by the laser penetrates the vagina to a depth of 0.5 mm, resulting in a 30% reduction in tissue volume. This, in turn, causes mechanical traction of the innermost layers, which further contributes to the adjustment effect due to the production of elastin fibres and the stimulation of neocollagenesis, leading to an increase in the thickness of the vaginal epithelium, and elasticity and firmness of the wall, which may be related to the restoration of urethral coaptation mechanisms involved that are impaired in the physiopathology of SUI [4].
Atrophy of the pelvic floor muscles and the reduction of collagen content may be important factors in the increased prevalence of both SUI and urge urinary incontinence (UUI). Laser-induced neocollagenesis can change the composition of the pelvic floor structures and, therefore, increase the pressure throughout the length of the urethra, including proximal urethral pressure. This increase in proximal urethral pressure can relieve overactive bladder (OAB) symptoms by reducing the reflex response of the bladder.
There are controversies and doubts regarding the efficacy and safety of the CO2 laser in urinary incontinence (UI). Therefore, this article reviews, and tries to clarify, the available data on the use of the CO2 laser in the different types of UI.
Methods
This article reviews the available data on CO2 laser therapy for the treatment of SUI and UI. A bibliographic search of PubMed was conducted, using keywords that included laser, CO2 laser, stress urinary incontinence and urge urinary incontinence. All the publications reviewed here were in English and were published in the last 10 years.
Results
Urinary incontinence
Urinary incontinence is an uncontrolled or involuntary loss of urine that can vary widely from the leakage of a few drops to abundant release [5]. The different types of UI include SUI, UUI and mixed urinary incontinence (MUI). Stress urinary incontinence is the most commonly diagnosed [5] and is reported as an involuntary loss of urine associated with physical exertion that generates an increase in intra-abdominal pressure, when the intravesical pressure is greater than urethral pressure as a result of a failure of the urethral resistance mechanisms [3]. This may be due to urethral hypermobility, where the mechanisms that support the urethra fail, causing it to descend from its correct anatomical position, and/or to an internal sphincter deficiency, where the closure of the urethral walls is not sufficient, resulting in a decrease in urethral resistance [6].
Urinary incontinence affects 15-55% of women [7] and the severity of symptoms increases with age. The condition has been shown to have a significant impact on the quality of life and sexual life of those affected, for a number of reasons, including urine leakage during sexual intercourse, nocturnal bed-wetting and fear of urinating in bed, as well as general embarrassment associated with this condition that can have far-reaching psychosocial consequences in the unfortunate patient [7].
The high prevalence of female UI in the general population has led to the exploration of various treatment options and techniques to help improve symptoms. These range from Kegel exercises and physiotherapy for pelvic floor rehabilitation to more invasive approaches, in the form of surgical treatment. Surgery may not be the optimal therapeutic option for all patients as it is often associated with multiple contraindications, such as use of anticoagulants by patients, urinary infection, the desire to become pregnant, as well as the patient’s general apprehension and concern regarding the risks associated with surgical procedures. Less invasive surgical techniques are relatively effective, but are still related to complications (bleeding, erosions, urethral injury, infection, chronic pain and urinary retention) in >15% of cases [8], while conventional surgery is related to risks of anaesthesia and high recurrence rates (25%) [8]. This therapeutic vacuum has stimulated research and development of minimally invasive energy-based devices, such as lasers, that could be used as an alternative treatment option to address UI in women more effectively.
CO2 laser and SUI
The first studies on SUI and CO2 lasers were performed in GSM, hence the main objective was not incontinence per se, but all the symptoms related to GSM. Pitsouini et al. [9] reported a clear improvement in scores on the International Consultation on Incontinence Questionnaire-Female Lower Urinary Tract Symptoms questionnaire (ICIQ-FLUTS) and on the International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form questionnaire (ICIQ-UI SF) after three laser sessions.
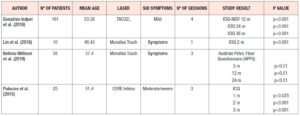
In 2018 González Isaza et al. [10] published a study of 161 postmenopausal patients with an average age of 53.38 years and mild symptoms of SUI. Four laser sessions were carried out, followed by three annual sessions, at 12, 24 and 36 months. The results showed a clear improvement in the ICIQ-UI SF score at 12 months (p<0.001), which was maintained at 24 months (p<0.001) and at 36 months (p<0.001) (Table 1). Subsequently, Lin et al. [11] performed a comparative study using an erbium laser in 21 patients and a CO2 laser in 10 patients. They only performed 1 laser session in patients diagnosed with SUI. Two months after the laser treatment, they found significant improvements on the ICIQ-UI SF, both in patients who received erbium laser (p = 0.007) and in those who received CO2 laser (p = 0.001) treatment (Table 1).
Recently Behnia-Willison et al. [12] found improvements in the Australian Pelvic Floor Questionnaire (APFQ) scores of 58 women diagnosed with SUI after three CO2 laser sessions. Significant improvements (p<0.01) were found in the results of this questionnaire at 3 months after treatment completion and the effect was maintained at 12 and 24 months (Table 1) .
Our group has just completed a study [13] in which there was a clear improvement in the moderate-severe symptoms of SUI after the first CO2 laser session (p<0.01), and the effect increased after the second (p<0.001) and third CO2 laser sessions (p<0.001) (Table 1).
CO2 laser treatment and UUI
Perino et al. [14] assessed the effect of CO2 laser treatment in postmenopausal women with UUI (>8 urinations/24 h) and >1 symptoms of GSM (itching, burning, reduced lubrication, superficial and/or severe dyspareunia) in the previous 3 months. The symptoms of OAB were evaluated using the abbreviated and validated form of the Overactive Bladder Questionnaire (OAB-Q SF). The results at a 1-month follow-up after the third laser session indicated a significant reduction in the number of urinations and the number of urge episodes (p <0.0001).
Clinical aspects
In the use of vulvovaginal laser treatment, which is simple and quick to perform, it is necessary to verify the absence of vaginal or urinary infections and ensure that, at the time of the treatment, the vagina is free of creams or gels, that is to say, it is dry. The procedure is virtually painless, well-tolerated, easily applied and effective. Usually, three procedures are performed, separated by intervals of between 4 and 6 weeks. The energy will depend on the device and the protocols established for each. However, treatment must be personalised, depending on the disorder to be treated, and the patient's age and sensitivity to the laser. 80% of women at the end of treatment are very satisfied/satisfied. Regarding tolerability, only 1 in 201 patients considered the procedure unacceptable, while tolerability was reported as excellent, good or acceptable in 90% of treated women. Less than 10% of patients referred to the procedure as a bad experience [2].
Although long-term safety concerns remain, it is expected that they may be resolved in the coming years as experience, in terms of the number of years in the same patient, validates the procedure. However, current experience indicates that if the protocols recommended by the various laser equipment manufacturers are followed, the procedure is very safe. The early detection of contraindications for use, as well as the individualisation of the energy applied and the number of sessions, will be key items of evidence.
In SUI, the indications for laser treatment must be understood. In other words, it must be understood that SUI is not only induced by urethral hypermobility, as a result of the weakening or alteration of the pelvic floor musculature and/or pubourethral ligaments, but is also due to weakening of the urethral sphincter. Women with urethral sphincter problems may not benefit from use of the laser, or at most may only experience an indirect benefit. However, the inclusion of women with mild to moderate SUI without prolapse should improve the results, especially the long-term results, of laser treatment. In short, the criteria for patient selection should be improved, and doctors should be aware that laser treatment may not be successful in a particular group.
Although there are few results on MUI and UUI, the data available give cause to be optimistic. Therefore, we await new studies that will confirm the therapeutic possibilities and provide more information on the possible mechanism of action.
Conclusions
In summary, the results of the available studies suggest that CO2 laser treatment for SUI and its symptoms provides an option for treating these pathologies and offers affected women a better quality of life. Data on SUI in premenopausal women are currently scarce and reported in the context of the syndrome of vaginal hyperlaxity, therefore we cannot draw conclusions. Most of the available data are in postmenopausal women with SUI. As for UUI, the data are very scarce and still inconclusive, so we will have to wait for new results.
The procedure is effective and safe if applied with the appropriate parameters. No serious adverse effects have been reported, or reports of adverse events have been anecdotal. However, more extensive, long-term and controlled studies with sham groups are required to explore the use of the vaginal laser to verify its efficacy and safety, refine protocols, and compare different therapeutic options.
Although these are simple and safe outpatient procedures, they must be used by experts who understand the female genital system, the indications, early detection of pathologies, and know how to personalise treatment with the specific protocols.
Declaration of interest
- none