Background
Among the main causes of declining reproductive function and performance in fertile women, uterine fibroids (UFs) play the most significant role. They are the most common benign tumours of the female reproductive system [1-3], consisting of myogenic elements and the stromal component of the myometrium [4].
Despite the development and availability of modern diagnostic and treatment methods, the prevalence of this pathology has been growing, affecting 35-50% of women over 35 years of age. Furthermore, according to histopathological results following uterine removal for various reasons, this rate may be even higher (up to 70-84%) [5,6].
Over the past twenty years, there has been a trend towards an increasing prevalence of this pathology in young women [7,8]. The average age at diagnosis is 32 years, a time of life when women are likely to be professionally and socially active. A survey of 968 women with UFs in the United States found that 28% lost their jobs due to fibroid symptoms, and 24% believe that this condition has become a barrier to their career development. Of those surveyed, 79% wanted non-invasive treatment, 51% wanted to preserve the uterus, and 43% wanted to preserve their fertility. These findings may explain the average treatment delay of 3.6 years [8]. The trend to delay reproductive plans, the burden of comorbidities, and the increase in the incidence of UFs with age together present clinicians with a real challenge.
We present a clinical case of UF treatment that lasted ten months. It required the use of hysteroscopy, the prescription of ulipristal acetate (UPA) and goserelin acetate, and uterine artery embolisation, which led to expulsion of the fibroid. After the treatment, pregnancy occurred, which ended with a live birth.
Case presentation
Patient K., 35 years old, came to the clinic on 05.01.2017 complaining of heavy, painful menstrual periods with prolonged spotting before and after menstruation, general weakness and dizziness in recent months, and pains in the lower abdomen. She had a 10-year history of infertility.
Gynaecological history: menarche at 12 years, menstruation lasting for 6-7 days, cycle duration: 28 days. The patient reported one pregnancy, which had ended in spontaneous miscarriage. Her height was 162 cm, her weight 74.3 kg, and her BMI 28.2 kg/m².
The patient had already sought medical help for a UF discovered a year previously, but the only treatment offered was a hysterectomy, which she categorically refused due to her desire to have a baby.
Investigation
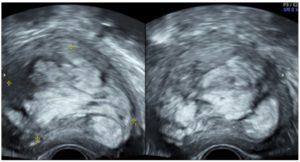
Transvaginal ultrasound examination (TV-US) of the pelvic organs, performed at the first visit using a Voluson™ E8 device, revealed a uterus with a volume of 205.19 cm³ (85.0х68.0х71.0 mm). Along the anterior wall of the uterus, a type 3 submucous UF was visualised, with a volume of 147.8 cm³ (63.0х51.0х92.0 mm). The UF showed pronounced peri- and intranodular blood flow, and a heterogeneous echo structure, taking the form of vortex-like lobules (Fig. 1). The endometrium was 5.4 mm thick, with a homogeneous echo structure. The ovaries showed typical location with clear and even contours. The right ovary measured 34.0x24.0x22.0 mm, and the left one 37.0x19.0x18.0 mm.
Clinical diagnosis: symptomatic uterine fibroid, adenomyosis.
Treatment
The patient wished to carry out conservative treatment with minimal use of surgical techniques. The fibroid was large, with a complex multi-component structure, and showed pronounced vascularisation. Thus, conservative myomectomy (CM) could have been complicated by bleeding. Furthermore, because of the atypical structure of the UF and its intramural-submucosal localisation, CM would have entailed multiple penetration into the uterine cavity, which was undesirable given the patient's reproductive plans. Therefore, UPA was chosen as the first-line treatment. Since the UF, due to its pronounced vascularisation, was causing heavy menstrual bleeding, hysteroscopy was a crucial stage of the treatment, in order to verify its benign nature prior to further treatment. Partial hysteroscopic resection of the UF was performed on January 24, 2017. As expected, increased tissue bleeding was observed during the procedure and afterwards (pelvic ultrasound showed perceptible blood flow). Tranexamic acid was prescribed in the postoperative period. Having received histopathological confirmation of the benign nature of the UF (uterine leiomyoma of normal structure with stromal hyalinosis and foci of adenomyosis; cyclic proliferative endometrium), the patient was prescribed UPA (Esmya®) 5 mg once a day orally for 3 months.
The plan was to perform a CM after reducing the size of the UF, or uterine fibroid embolization (UAE) should the Esmya® not be sufficiently effective.
TV-US was performed two weeks after hysteroscopy during the treatment with UPA (Esmya®). The uterus measured 176 cm3 (73.0x71.0x68.0 mm), and the node 59.6 cm3 (54.0x46.0x48.0 mm). Thereafter, resection of the node was performed, reducing its size by 32.2%.
Menstruation occurred one month after completing the three-month course of Esmya. The patient had a follow-up examination. The results of TV-US were disappointing. The volume of the uterus appeared to be 376 cm3 (93.0х91.0х89.0 mm), while the volume of the UF was 139 cm³ (82.0х53.0х64.0 mm). Paradoxically, the UF had continued to grow, increasing by 44.94%. It was decided to perform UAE, considering the pronounced vascularisation of the UF and the woman's continued desire to preserve the uterus and give birth.
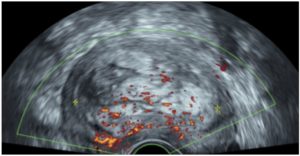
UAE was performed on June 15, 2017. However, one month after the procedure, the volume of the uterus appeared to be 312 cm³ (90.0х78.0х89.0 cm), and the volume of the UF was 129 cm³ (77.0х55.0х60.0 mm). Contrary to our expectations of absence of blood supply to the UF, marked peri- and intranodular blood flow was visualised on colour Doppler imaging (Fig. 2.) This indicated the ineffectiveness of the treatment, with the UF size increasing by an additional 34.52%.
Considering the features of the UF (size, submucosal localization, pronounced intranodular blood supply), as well as the ineffectiveness of conservative and minimally invasive treatment, laparoscopic CM was proposed. In view of these features, a GnRH agonist (goserelin, 10.8 mg) was used, administered subcutaneously. Goserelin was expected to create the conditions for safer surgery and to reduce the risk of intraoperative blood loss.
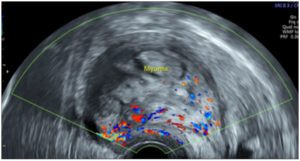
Two months after goserelin injection (07.09.17), the patient was invited for an examination before surgery. The patient had no complaints. She experienced neither lower abdominal pain nor bleeding or spotting. On TV-US, the volume of the uterus was 214 cm³ (83.0х70.0х74.0 mm), while that of the UF was 118 cm³ (72.0х60.0х55.0 mm); the examination showed pronounced intra- and perinodular blood flow; the uterine cavity was filled by the UF that was found to have become elongated and spindle shaped, with a heterogeneous structure.
Partial expulsion of the node into the uterine cavity, with its prolapse into the cervical canal, was observed (Fig. 3). Therefore, UF of type 3 had transformed into type 2. The feasibility of laparoscopy was now questionable.
Expulsion symptoms were not observed. There was neither cramping pain in the lower abdomen nor discharge from the genital tract. Body temperature was not elevated. Therefore, it was decided to choose expectant tactics with prolongation of drug-induced menopause. In the event of spontaneous expulsion or vaginal UF extraction, the formation of a scar on the uterus is excluded, which is a favourable factor for a future pregnancy.
One month later, the patient complained of constant pain in the lower abdomen, which during the last 24 hours had acquired a cramping character; she also reported minor spotting. Her body temperature was 37.0 C at the time of examination. During the vaginal examination, the cervix appeared soft, shortened to 2 cm, and the external os of the cervical canal was opened to 3 cm, where the UF tissue was prolapsed.
According to TV-US, the uterus volume was 273.4 cm³ (81.0x75.0x90.0 mm), while that of the UF was 117 cm³ (72.0x62.0x54.0 mm). The cervical canal was dilated to 23.0 mm and contained UF tissue.
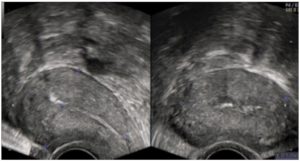
The patient was hospitalised. On October 18, 2017, when the cervix was 5.5 cm dilated, the UF was removed with further hysteroscopic revision of the uterine cavity. Macroscopically, the uterine fibroid displayed the peculiar lobular irregular structure previously visualised on TV-US. The UF showed no signs of decay (Fig. 4).
Postoperatively, the patient was prescribed antibacterial and symptomatic treatments. She was also prescribed Qlaira®, 1 tablet a day, according to the usual scheme, for 6 months. The aim was to ensure contraception during the period of myometrium restoration before pregnancy planning.
According to TV-US, one month after the expulsion of the UF (29/11/2017), the uterus measured 54.0x38.0x49.0 mm. The structure of the myometrium was echo-homogeneous; the uterine cavity was neither deformed, nor dilated (Fig. 5).
Observation was recommended once every 3 months. It is recommended to plan pregnancy no earlier than 6 months after expulsion of a UF.
Outcome and follow-up
The patient became pregnant spontaneously. On 16/08/2019, TV-US showed early-stage pregnancy.
The pregnancy was complicated by cervical insufficiency. A circular suture was placed on the cervix, and a pessary was installed. On April 13, 2020, an urgent caesarean section was performed. The pregnancy was complicated by severe preeclampsia at 37-38 weeks of gestation. The woman gave birth to a boy (50 cm, 2500 gr).
Six months after the birth, LNG IUD (Mirena®) was inserted.
Discussion
Today, a wide variety of organ-preserving methods in UF treatment allow patients to preserve not only the uterus as an organ, but also its reproductive function. The availability of a sufficient number of non-invasive or minimally invasive methods of UF treatment makes it possible to choose the best method based on the clinical situation as well as the patient's wishes.
This patient, like many others [9], was looking for a treatment that would not deprive her of her chance of conceiving. Having refused hysterectomy, she hesitated to start treatment.
Considering the location and size of the UF (FIGO type 3, diameter 6.3 cm to 9.2 cm), it was impossible to carry out hysteroscopic resection, even in several stages. However, hysteroscopy was necessary to verify the benign nature of the UF before treatment with UPA (Esmya®). Despite the fact that detection of leiomyosarcoma is a rare event - it is detected during the primary treatment of uterine fibroids in 0.13%-0.29% of cases [10] - an important part of fibroid treatment is its differential diagnosis with this malignant tumour, as well as the examination of the endometrium.
Unfortunately, the use of UPA was ineffective in this case and the fibroid continued to grow. According to the latest systematic review and meta-analysis, published in 2021, UF size reduction during treatment with UPA occurs in only 56.5% of cases [11].
Fortunately, in the present case, a histopathological study confirming the benign nature of the node allowed us to continue our treatment attempts.
Eventually, it was decided to perform UAE, considering the pronounced blood flow in the UF. However, this too proved ineffective. Not only was the blood flow in the fibroid preserved, but the fibroid continued to grow.
The reasons for this phenomenon can only be guess at. Perhaps there was atypical vascularisation: the UF had several vascular sources, including alternative vascularisation (anastomosis with the ovarian artery, which was not noticed or visualised on fluoroscopy during UAE) [12]. Another possible reason could have been a spasm of the uterine artery when irritated by an endovascular catheter. Or it may have been caused by the vortex-like structure of the fibroid tissue. According to a study by Jayes et al., heterogeneity of structure, collagen content, and density may be associated with biomechanical signalling and variations in UF growth [13].
Considering the size, localisation, and pronounced blood supply of the UF, as well as the ineffectiveness of medical and minimally invasive treatment, it was proposed to conduct laparoscopic CM. In order to reduce blood loss during surgery and to reduce the size of UF, goserelin 10.8 mg was administered subcutaneously [14].
A month later, the patient complained of cramp-like pains in the lower abdomen. The examination revealed further dynamics of the expulsion, and the UF was excised during hysteroscopy. Antibiotic prophylaxis was administered. For a period of 6 months, the combined oral contraceptive Qlaira® was prescribed for contraception to restore myometrial function before pregnancy. According to the latest publications, UAE is accompanied by fibroid expulsion in 3-15% of cases [15]. However, there are no proven pathogenetic mechanisms that can explain why fibroids migrate to the uterine cavity. There is a single study that shows that the likelihood of migrating is higher when the minimum distance to the endometrium is less than 2.4 mm and the maximum UF diameter is larger than 5.1 cm (measured by MRI) [16].
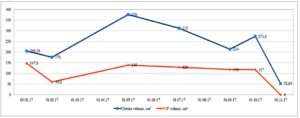
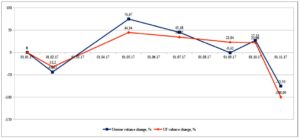
As a result, in one month the uterus looked normal on TV-US, and the uterine cavity was not deformed. Therefore, it took 10 months to treat this uterine fibroid. The dynamics of changes in the size of the UF and the uterus are shown in Graphs 1 and 2.
Treatments with UPA, UAE, and a preoperative GnRH agonist were used, resulting in expulsion of the fibroid. It took 1 year and 4 months (not including the 6 months of contraception) for a spontaneous pregnancy to occur after the treatment, which is a little longer than for healthy women in the population.
UAE is thought to have a negative impact on fertility and is not recommended for nulliparous women. However, the latest data, including the recent systematic review and meta-analysis by Ghanaati et al., indicate that the incidence of obstetric complications, pregnancy loss, and preterm births after embolisation is comparable to population data [17].
Six months after delivery, the patient’s periods returned, moderate and painless, and LNG IUD Mirena® was installed for contraception.
Funding
We have no financial relationship to disclose.