Introduction
Current contraceptive methods, namely those based on hormonal contraception, really came to prominence in the 1960s, after Gregory Pincus and his colleagues published the first clinical trials in women on norethisterone and norethindrone, used to inhibit ovulation [1]. Contraceptive methods are commonly categorized as natural, barrier methods, short-acting hormonal forms of contraception, long-acting reversible contraception, and irreversible methods [2]. In this review, we aim to provide a comprehensive overview of the different contraceptive modalities, outlining their benefits and downsides, with a historical context.
The Pearl Index
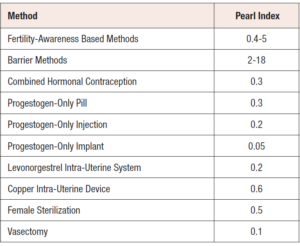
The Pearl Index, named after the American Scientist, Raymond Pearl, is one of the objective ways of measuring the efficacy of contraceptives. The lower the Pearl Index, the more effective the contraceptive method tends to be [2,3]. The Pearl Index is expressed as the contraceptive failure rate per 100 women years of use, assuming perfect usage. Therefore, if 100 women, use the same contraceptive for one year and one pregnancy occurs during this period, the Pearl index is one [2,3]. The Pearl Indices for the contraceptives discussed in this paper are shown in Table 1. Unfortunately, the Pearl index is hampered by a number of limitations. The number of unintended pregnancies observed by a given contraceptive method tends to decrease over time as most of the contraceptive failures happened earlier during such studies and such women exit the study at an early stage, leaving a selective cohort of highly motivated women. Therefore, the Pearl Index is not suitable for assessing contraceptive failure rate, between two different studies carried out across different time intervals [4].
Natural methods of family planning
This includes the natural fertility-awareness based methods, coitus interruptus and sexual abstinence. The fertility awareness-based methods, as the name implies, involves teaching the couple, to identify a woman’s fertile period either by observing the changes in cervical mucus (the Billing’s method), palpating the cervix for changes in its position or consistency, measuring the basal body temperature and identifying the 0.2°C rise associated with the progesterone surge following ovulation (the symptothermal method) as well as calculating the days when a woman is most fertile from the calendar according to her cycle length (the calendar method) [5]. The couple is then advised to abstain having sexual intercourse, whenever these signs indicate that a woman is fertile. These indicators can be used either alone or in combination. The acceptability to use, sexual abstinence and coitus interruptus, depends very much on the meaning given to it, by people from different cultures and can be quite unreliable methods of contraception, especially where young people are involved [5-7]. The advantages of natural family planning methods are that they are cheap, readily acceptable to most religious beliefs and free from any side effects. Unfortunately, they are highly user-dependent and cycles may sometimes vary in length, making it difficult to ascertain the fertile period, hence, rendering these methods not quite a reliable means of contraception [5].
The barrier methods
These include, male condoms, female condoms, caps and diaphragms. The use of male condoms is widespread, despite complaints of discomfort, abrasiveness, and chafing caused by contact dermatitis in the woman [8]. Condom use depends on correct application, good quality brands and reliable use [7,8]. The Pearl Index quoted is between 2-18 per 100 women years [9,10]. Condoms are more effective when used in conjunction with a spermicidal gel. Female condoms or caps, which are smaller than male condoms, are also available and are user-dependent just as their male counterparts. They are also recommended to be used with a suitable spermicidal gel for maximal effectiveness [7,8]. The added advantage of barrier contraception is that it is the only contraceptive modality that protects against sexually transmitted infections [9].
Short-acting hormonal contraception
The Combined Oral Contraceptive Pill (COCP)
It has been over 60 years, since the combined oral contraceptive pill (COCP) was introduced. The basic principles have remained unchanged in the monophasic preparations, which combine the same dose of both an estrogen and a progestogen, for 21 days with 7 days off [1,11]. Most preparations contain, the synthetic 17β-ethinylestradiol (EE), normally at 30 micrograms per day but doses vary according to the COCP from 15 micrograms per day to 35 micrograms per day [12,13].
The estrogen in the COCP is combined with a progestogen. Natural progesterone is broken down rapidly in the stomach and gastrointestinal tract. Although, a micronised form of oral natural progesterone exists, this is not considered sufficient in dosage so as to be tolerated, or reliable enough to be used in an oral contraceptive pill. A variety of progestogens have therefore been developed.
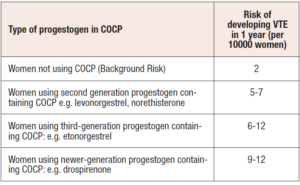
The progestogens also vary in terms of their androgenic properties, from strongly androgenic ones, right across to anti-androgenic ones. This variation includes cycle stability properties, or cycle effects such as acne, mood change or bloating [12,13]. Unfortunately, there was an associated slightly increased risk in venous thromboembolism (VTE) associated with the newer-generation progestogens such as drospirenone [14]. The risk of VTE associated with different progestogen subgroup components in the COCP are shown in Table 2. The general consensus is to prescribe a COCP containing drospirenone, only when its anti-androgenic benefits are desired such as for instance in women with polycystic ovarian syndrome [14]. Otherwise, if the clinical indication for COCP use is contraception, use of a COCP containing an older generation progestogen is preferable. Few brands of COCP contain an anti-androgen, and this contributes to controlling pre-existing conditions of hyperandrogenism, acne and hirsutism [12,13].
Estrogen dose
The estrogen dose in the combined pill has been reduced through the years, in an attempt to reduce cardiovascular risks. Very low dose COCPs, however, are associated with increased breakthrough bleeding and are very often taken for 24 or 28 days instead of the traditional 21-day regimens [12,13].
There has also been the introduction of using 17β estradiol (E2) itself and estradiol valerate. These ‘natural’ estrogens improve the metabolic effects of the usual COCPs and reduce thromboembolic risk often associated with 17β EE. The risk of breakthrough ovulation is reduced with a reduced pill free interval (24 days on and four days off the cycle) [12,13].
Sometimes, COCPs, can be prescribed back-to-back, with no pill free interval, for any period from 2-3 months to a whole year, at a time. This will help reduce the risk of escape ovulation usually caused by missed pills [11]. A meta-analysis showed that women on continuous or extended combined hormonal contraception regimens fared better in terms of frequency of occurrence of pre-menstrual symptoms than the cyclical combined hormonal contraception group [15]. The most common complication of ‘back-to-back’ use of oral contraceptive pills, is breakthrough bleeding and amenorrhoea [12,13].
The latest addition to the COCP armamentarium is estetrol-containing contraceptives. Estetrol is a type of estrogen that is produced solely by the fetal liver. It only activates nuclear receptors as opposed to the membrane ones and in so doing it only exerts its effects at specific target organs and tissues [16]. In particular, it has been shown that it has a strong estrogenic effect on the ovaries and uterus, whereas minimal to no effect on the breast and liver leading to reduced risk of breast cancer, thromboembolic disease and hypercholesterolaemia compared with older generation estrogens [16].
The role of progesterone in the contraceptive effect of the COCP
In contraceptive formulations, the progestogen is primarily responsible for preventing pregnancies. Progestogens inhibit follicular development and prevent ovulation. Progestogens provide a negative feedback to FSH/LH production and results in a lack of estrogen production. This lack of estrogen production, furthermore, prevents a mid-cycle LH surge, that is essential for ovulation [12]. The estrogenic component of a COCP, furthermore adds to competitive inhibition of follicular development since it interrupts the ovarian pituitary feedback loop. Thus, estrogen exacerbates the progestogenic effect in inhibiting ovulation. Progestogens also affect cervical mucus rendering it hostile to sperm [12,13].
Variations in formulation of hormonal contraception
The vaginal ring is a combined estrogen-progestogen pessary that is inserted vaginally and replaced every 3 weeks with a one-week break [17,18]. A randomized open-label study comparing the combined contraceptive vaginal ring to the COCP, showed that the former was associated with a slightly reduced risk of breakthrough bleeding [19]. It releases 15 micrograms of 17β EE, and 120 micrograms of etonorgestrel per day [19]. By continuously releasing the sex steroids, in a regular manner, it has been shown to be an efficacious form of contraception [17,18]. Like the COCP, the combined vaginal ring is a form of systemic hormonal contraception and therefore has the same risks including VTE as the COCP. There is some evidence to suggest that the risk of VTE may be higher in the non-oral formulations [7]. This is possibly due to its sustained continuous absorption into the bloodstream and its long half-life.
Non-contraceptive benefits of combined hormonal contraception
There are many reasonably to well established non-contraceptive health benefits related to oral contraceptive use. The COCP has been associated with a reduction in menstrual disorders, dysmenorrhea, benign breast disease, pelvic inflammatory disease, ectopic pregnancy, protection against endometrial, ovarian and colorectal cancers, a potential reduction in endometriosis, less rapid progression in rheumatoid arthritis as well as improvement in bone mineral density [12,20-22].
The progestogen only pill (POP)
As the name implies, this form of contraception involves, a daily oral progestogen dose, taken continuously [23]. The mini-pill, as it is known, is an oral contraceptive that contains only a progestogen, a synthetic, progesterone-like molecule. There are different types of progestogen, with different preparations, but all formulations mimic the function of progesterone, in the menstrual cycle [23,24].
The POP is thought to exert its effect through rendering the cervical mucus hostile to sperm. There could also be, suppression of ovulation, but this is not consistent [25]. In a prospective, randomized cross-over study carried out in the United States, in which women used a POP of 0.075 mg norgestrel for three 28-day treatment cycles and were followed up with ovarian ultrasonography and reproductive hormone measurements, two thirds of patients had suppression of ovulation, whereas, out of the third of patients that ovulated, a third of them had an abnormal luteal phase [26]. A POP needs to be taken every day in order to prevent escape ovulation that might lead to a pregnancy [23,24]. The POP is recommended during breast feeding [27], although contrary to popular belief, the COCP does not inhibit lactation. The POP is contraindicated in women who have had breast cancer, liver disease, unexplained uterine bleeding, and in women who are uncompliant to oral medication [21,25,27].
The failure rate of women on the POP is higher than those on COCPs reaching 1 to 7 out of 100 women years regardless of whether these are taken at the same time of the day or not. As with intrauterine contraceptive devices (IUCD) there seem to be a higher rate of ectopic pregnancies. Side effects from the POP include irregular menstrual bleeding, acne, breast tenderness, loss of libido, psychological neurosis e.g., depression, headaches, nausea, ovarian cysts and bloating [24].
The POP should be started in the first five days of the menstrual cycle. After birth one normally recommends starting between 3- and 6-weeks post-partum. When switching to a COCP, one can start on the very next day after stopping the POP [24].
Types of POP
The POP comes in a pack of 28 pills. Although there are many brands of POPs, they are all the same dose throughout the cycle, and contain the same active ingredients. There are two principal ones used, one contains norethisterone 350 micrograms and the other contains desogestrel 75 micrograms.
Benefits of POPs
POPs are an effective birth control pill and a substitute in women who cannot take a COCP. Apart from birth control, POPs may also be beneficial in alleviating menstrual symptoms, cramps, and endometriosis. Taken every day, POPs may protect against endometrial cancer [17,25].
Disadvantages of POPs
Spotting or breakthrough bleeding can last for a few days after starting the POP. Some women can also become amenorrhoeic. Symptoms of acne, mood swings, nausea, dizziness, bloating, weight gain and headaches tend to be also common. Cardiovascular disease risks tend to be associated with COCP use, but also to a lesser extent with POP use, including deep venous thrombosis, myocardial infarction, and stroke [21,22,25]. However, this is debatable as a systematic review has shown that there is no evidence available that suggests an increased risk of cardiovascular events such as VTE, stroke or acute myocardial infarction with progestogen-only contraception [28]. The possible association of contraceptive use with breast cancer continues to be debated, with conflicting results being reported. A large, population based, case-control study in the United States analyzed the risk of breast cancer among women aged 35 to 64 years [29]. The results showed that neither current, nor past use of oral contraceptives, increased the risk of breast cancer, compared with population-based controls. The results did not vary according to the number of potential risk factors, such as estrogen dose, duration of use, family history of breast cancer or time of initiation of use. The conclusion of this study indicates that breast cancer risk related to oral contraceptive use appears to be negligible in most women [29].
Long-acting reversible contraception
The IUCD together, with other contraceptive modalities such as the progestogen implant and the progestogen injection, form part of a category of contraceptives named long-acting reversible contraceptives (LARCs) [30]. The main features, shared by these contraceptives are that they provide a form of contraception which is not user-dependent, lasts for months or years on end and can be easily reversed.
Intrauterine contraceptive devices (IUCDs)
IUCDs are commonly used and date back to over a century, but the original concept is said to have come from Bedouins taking their camels on long desert journey and thus not desiring a pregnancy during their caravans [31].
The first IUCDs were not easily retrieved. The Grafenberg ring would be inserted into the uterus, and this was an effective method of contraception. Later, retrievable plastic devices were developed starting with the Lippes Loop. Copper was added to the devices leading to the popular copper T or other variables along these lines [31].
Finally, came the medical devices with slow release levonorgestrel in the stem and this gave rise to the intrauterine medical devices. There are variations of such devices. These devices release a low dose of levonorgestrel and are more effective than other IUCDs, in disrupting the cervical mucus so as to render the mucus hostile to sperm and preventing fertilisation. The endometrial environment is also altered with endometrial thinning occurring [30]. A secretory type of endometrial histology prevails with the levonorgestrel devices. Menstruation is also less heavy compared to normal [30]. This is not the case with the copper and plastic only devices where the endometrium is also disrupted. The levonorgestrel devices, like the POP can prevent ovulation.
Coil failures are commoner with the non-medicated devices. There is also a slightly increased risk of ectopic pregnancies with IUCDs. Even though, the background risk of pregnancy is reduced, if pregnancy occurs it is more likely that such pregnancy is an ectopic one. Since there seems to be no protection against ectopic pregnancies in these cases particularly in primigravids, non-medicated IUCDs carry a higher risk of pelvic inflammatory disease [20]. The main advantage of the IUCD is that patient compliance is much better and contraception is available continuously and reliably, throughout its use. More recently, contraceptive efficacy of the 52 mg levonorgestrel intra-uterine system has been shown to last up to 8 years in the Mirena extension trial [32].
The progestogen implant
Amongst the types of contraceptive implants available are Implanon (etonogestrel) and the Norplant/Jadelle system (levonorgestrel) [33]. Implanon is used to prevent pregnancy for up to 3 years, whereas Norplant is used to prevent pregnancy for 5 years. Implanon (etonorgestrel) is in the form of a plastic rod that is implanted into the skin of the upper arm. The rod should remain in place and provide continuous contraception for up to 3 years. The Norplant system contains levonorgestrel. It consists of six (6) plastic rods each containing 36 mg of levonorgestrel and is injected in a similar fashion. Jadelle is a newer version marketed with a silastic rod and is similar to Implanon [33].
Advantages of contraceptive implants
The advantages of contraceptive implants are, that they offer highly effective contraception within 7 days of insertion. They are relatively inexpensive and safe, and they can easily be removed, should the woman desire to become pregnant. They are not user-dependent, in stark contrast to the COCPs. Contraceptive implants are also safe to use in lactating mothers [27]. Menstrual control is better and offer an alternative to the Mirena coil in relieving menorrhagia or dysmenorrhea.
Disadvantages of implants
The disadvantages of progestogen implants are very similar to the disadvantages of all unopposed progestogen preparations including the levonorgestrel intra-uterine system. Rarely, there are some problems with insertion, such as bruising, migration of implant and a broken or bent implant. Removal of the implant is a simple procedure which can be carried out in the clinic under local anaesthesia. This would involve a small incision near the distal tip, which then allows the implant to be pushed out from the other end through the incision [33].
Contraceptive progestogen-only implants operate through suppressing ovulation. There are also changes in the cervical mucus that make it viscous, scanty, and impenetrable to sperm. No sign of embryonic development has been found amongst implant users indicating that the implant lacks abortifacient properties [20].
Injectable contraceptives
The main type of injectable contraceptive that has been used for a few decades is depot medroxyprogesterone acetate (DMPA). This is, in the form of quarterly injections given intramuscularly and provides a highly reliable form of contraception. Its advantages are its reliability and lacking user-dependency. Its main disadvantages are that it is associated with a decrease in bone mineral density [7,34] and there have been studies showing a possible increased risk of breast cancer in DMPA users [35]. The mode of action is similar to the POP, progestogen implants, or the levonorgestrel intrauterine system (Mirena IUS) [18].
Irreversible contraception
Irreversible contraception consists of a vasectomy in men and tubal ligation in women. A vasectomy is rarely reversible and even if reversed, the sperm counts tend to be low. Apart from some bruising and soreness, this is a straightforward procedure. However, sterility has to be confirmed by submitting a semen sample about 4-6 weeks after the procedure. Meanwhile, the use of other contraceptive methods is advised [36].
In women, a tubal ligation, division, or salpingectomy, can be carried out as a form of irreversible contraception. This can be carried out, laparoscopically via a mini laparotomy or at the time of caesarean section. This is an irreversible form of contraception, in which the tubes are occluded such that they cannot transport the female oocyte from the ovary to the ampulla where it is fertilized. However, ovulation continues unchecked. Both forms of irreversible contraception demand proper counselling [36].
Emergency contraception
Any form of emergency contraception should be administered within 72 hours of unprotected sexual intercourse (UPSI). The oldest used method consisted of 2 pills of 17β EE 50 mg, followed by another 2 pills 12 hours later. An alternative to this would be 4 pills of 17β EE 30 micrograms followed by 4 pills 12 hours later [37]. Oral emergency contraception on the market, typically consists of levonorgestrel 1.5 mg which should be taken within 72 hours of UPSI. The latest evidence from a randomized double-blind placebo-controlled trial suggests that the efficacy of levonorgestrel as an emergency contraceptive can be enhanced by co-prescribing it with a cyclo-oxygenase – 2 inhibitor [38]. Other preparations, consist of mifepristone 600 mg administered within 72 hours of UPSI. Selective progesterone receptor modulators (SPRMs) such as ulipristal acetate can also be used [37].
Ulipristal acetate (UPA) should be taken within 120 hours (5 days) after UPSI. Orally-administered UPA, for the purposes of emergency contraception is available, as a single dose of 30 mg [39,40]. Both UPA and levonorgestrel work by inhibiting ovulation and hence are most likely to be effective if taken as soon as possible after coitus. The most common side effects are headaches, nausea, abdominal and upper abdominal pain. Finally, the copper intra-uterine device (IUD), inserted as early as possible after unprotected coitus, but not later than 5 days can also be of use [40].
The effectiveness of both forms of oral emergency contraception is limited in a woman with an increased body mass index. It is also ineffective if vomiting occurs within 3 hours [39,40], in which case, another dose should be prescribed, or an IUD fitted. UPA has been described as lowering the chance of pregnancy by 85% if taken as instructed [39].
Conclusion
In the 90 years or so, since the beginning of the current era of contraceptive cover, the basic pattern of preparations in use, to prevent unwanted pregnancies has remained by and large the same. This was a major stride forward in improving the general health of mothers, children, and their families. These methods have proven to be both safe and efficacious if used properly and have led to a considerable improvement in living standards. Undoubtedly, however, the downside has been a reduction in the younger population, mostly in western countries. Future developments will continue to concentrate on ease of use and efficacy of treatment.
Conflicts of interest
The authors declare having no conflicts of interest.