Introduction
Hysteroscopy, a frequently used tool in the diagnosis of infertility [1,2], is safe and easy to perform. Nonetheless, it is an invasive procedure, even when performed in an outpatient setting [1,2]. Thus, one should get the maximum informative output [3]. In the last decade, several methods for the evaluation of Fallopian tube patency using diagnostic hysteroscopy have been published [3,4].
Among them, the bubble or “Parryscope” technique has been claimed to be most promising, since it is easy to use and highly reliable [3-7]. The method involves provoking an infusion of a small amount of air bubbles into the uterine cavity during hysteroscopy and observing whether these would traverse the (patent) ostia [5-7]. Using this method, every Fallopian tube can be assessed separately. Despite an observed sensitivity of up to nearly 98%, specificity ranges from 69.5 to 83.7% for tubal patency measured by laparoscopic chromopertubation in an initial study [5]. In another study, the sensitivity was about 90%, whereas the specificity was 100% [6]. However, this implies that the overall accuracy would not reach 100%.
Concerning tubal patency, the most disastrous circumstance for a woman wishing to get pregnant is bilateral occlusion. Thus, it would be of clinical relevance to diagnose women in this situation as accurate as possible. It has been reported that the sonographic evaluation of pre- to post-hysteroscopic changes in cul-de-sac (CDS) fluid volume would predict bilateral occlusion in a highly reliable manner [8-13]. In detail, a fluid shift will be detectable in case of at least one open tube. Vice versa, the lack of fluid accumulation in the pouch of Douglas would suggest bilateral occlusion.
Although observing changes in CDS fluid volume was used in addition to the bubble technique in the original study of Parry et al. [5], it is still unclear to what extent the simultaneous application of both methods would increase the accuracy for the ruling out of bilateral occlusion. We aimed to analyze this in our retrospective cohort of infertile women, who underwent diagnostic hysteroscopy followed by laparoscopy with chromopertubation. In all women, both the “bubble sign” (also called ”Parryscope” method) and pre- and post-hysteroscopic transvaginal ultrasound measures for the detection of changes in CDS fluid volume were applied.
Methods
Patient population
In a previous prospective study, 115 subfertile women, who underwent combined hysteroscopy and laparoscopy (March 2018 - November 2019), were included and the predictive value of peri-hysteroscopic changes in CDS fluid volume for tubal patency was tested [8]. In 95 of these patients, the “bubble sign” was also tested, which allowed a secondary analysis of these cases.
The study design has previously been described [8]. In short, the following inclusion criteria had been applied: women with subfertility, age 18-44, scheduled for hysteroscopy and laparoscopy with chromopertubation. Women who had undergone removal of one or both tubes were not eligible for the study. All participants had signed a written informed consent prior to the operation. The study had been approved by the Institutional Review Board of the Medical University of Vienna (IRB number 1096/2018).
Surgical technique
Concerning the surgical technique, details have also been published previously [6,8,13,14]. Notably, all surgical procedures were conducted in an inpatient setting under general anesthesia. Experts in infertility surgery either directly performed or supervised all procedures. For hysteroscopy, a forward-oblique 30° hysteroscope (Karl Storz GmbH & Co KG, Tuttlingen, Germany; sheath diameter: 5 mm) was used. Continuous inflow of an intravenous solution of 0.9% sterile saline was generated with tubing with a drip chamber, and a reusable IV pressure bag. The minimal amount of inflow which resulted in sufficient uterine distention was used.
After hysteroscopy, we measured intrauterine length, defined as the distance from the uterine fundus to the external cervical os. As the next step, a “Spackmann” uterine manipulator with clamp fixation and a rubber cone (Reference number 1264; WISAP ® Medical Technology GmbH Brunnthal/Hofolding, Germany) was placed through the cervix (with a distance of one centimeter from the uterine fundus for each patient) [8,10,13]. During the laparoscopy, a 50 mL syringe with a dilute solution of indigo carmine blue dye (Amino AG Gebersdorf, Switzerland) was injected through the uterine manipulator for chromopertubation.
Assessment of tubal patency
For the air bubble technique, about 0.25 mL of air was introduced into the intravenous tubing by inverting the drip chamber to create bubbles. When air entered the uterine cavity, a single, large air bubble (extending fully from the anterior to the posterior wall of the uterine cavity) or stream of air bubbles traversing the ostia was considered suggestive of tubal patency. Notably, intracavitary evaluation was typically performed for at least ten seconds before air bubble entry since this is believed necessary for pressure equilibration in case of a hydrosalpinx. If patency was not observed, a minimum observation period of 30 seconds per ostium was performed [5,6]. Details about this technique can be watched online in a video by Dr. Parry (https://youtu.be/HU3MnxdK2o0).
For sonographic assessment of fluid in the Douglas pouch, transvaginal ultrasound was performed directly before and after hysteroscopy. This was done using an Aloka Prosound 6 ultrasound machine (Wiener Neudorf, Austria). We measured the fluid pockets located in the vaginal rear fornix, as previously characterized [8]. In detail, the sagittal field was used to measure the longitudinal length, whereas the coronal field was used to measure the diagonal dimension and depth length of the fluid pocket. Fluid volumes were calculated using the following formula: V (volume) = ¼ d1 (longitudinal measurement) *d2 (transverse measurement) *d3π (perpendicular measurement)/6 [8].
For the combined method (“bubble sign” + “peri-hysteroscopic sonography), bilateral tubal patency was suspected, if either both tubes revealed a negative “bubble sign” or if there was no increase in CDS fluid volume after hysteroscopy.
Parameters analyzed
The parameters assessed were documented by the senior surgeon using a prospective case report form. Hysteroscopic findings were entered into the form directly after hysteroscopy. Laparoscopy was performed by an independent surgeon blinded to the results of the hysteroscopic tubal patency testing. All outcomes were always supervised by a study member who was not part of the surgical team for each corresponding operation.
The main outcome parameter was tubal patency diagnosed by laparoscopic chromopertubation. In addition, the main focus was on hysteroscopic tubal patency testing, namely the presence of a sonographic fluid shift in the Douglas pouch before and after the hysteroscopy and a unilateral or bilateral positive bubble effect, which were both considered suggestive for patency of at least one Fallopian tube.
Other recorded parameters included: hysteroscopically diagnosed abnormalities in the uterine cavity; information about further laparoscopic surgical interventions; full uterine length; patient’s age and body mass index (BMI), the type of infertility (primary versus secondary); and the surgical indication. The AKIM software (patient management system at the Medical University of Vienna based on SAP ERP Release 2005, V33 01/2021; (Walldorf, Baden Würtenberg, Germany) was used for data acquisition, after data were collected and documented via prospective case report form and an Excel ®-table.
Statistical analysis
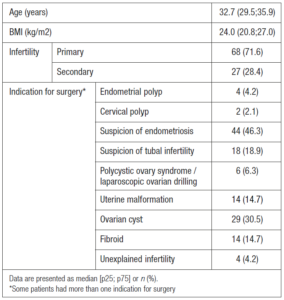
Data analyses were conducted using SPSS software 24.0 (SPSS Inc, 1989–2018). Numerical data are reported as median and interquartile range (IQR), while categorical data (primary/secondary sterility, indication for surgical intervention, abnormalities in the uterine cavity in hysteroscopy, tubal patency in chromopertubation, information about further laparoscopic interventions during the operation) were reported as number and percentage. Sensitivity, specificity, the positive predictive value (PPV) and the negative predictive value (NPV) including the 95% confidence intervals (95% CI) were calculated for the prediction of uni/bilateral tubal patency (versus bilateral occlusion). P values <0.05 were considered statistically significant.
Results
Basic patient characteristics are provided in Table 1. The operations were performed in the first half of the menstrual cycle in 86 patients (90.5%). There were no surgical complications. During hysteroscopy, bilateral tubal occlusion was suspected in 19 (20.0%) and 31 (32.6%) women using the bubble technique and peri-hysteroscopic sonography, respectively. After peri-hysteroscopic sonography, diagnostic hysteroscopy and post-hysteroscopic sonography, operative hysteroscopy had to be performed in 12 cases (12.6%) and a curettage in 6 patients (6.3%).
During laparoscopy, bilateral tubal occlusion was found in 19 women (20.0%) using the gold standard, namely laparoscopic chromopertubation. The respective cross-tabs for uni-/bilateral tubal patency using hysteroscopic methods of tubal evaluation can be found in Table 2. In detail, the hysteroscopic “bubble sign” predicted that at least one tube was open with a sensitivity of 94.7% (95% CI: 87.1-98.5) and a specificity of 78.9% (95% CI: 54.4-93.9; p< 0.001). In contrast, when a measurable increase in CDS fluid was detected sonographically, a sensitivity of 83.8% (95% CI: 72.9-90.7) and a specificity of 100% (95% CI: 78.1-100) were found for uni- or bilateral tubal patency (p<0.001). Last but not least, when both techniques were combined and patency of at least tube was only assumed when both hysteroscopic signs suggested this, sensitivity and specificity were 80.3% (95% CI: 68.5-87.6) and 100% (95% CI: 78.1-100), respectively (p<0.001).
Obviously, the combined assessment does not improve the accuracy. Given the fact that a positive CDS fluid shift was associated with uni- or bilateral patency in 100% and that in case of absence of such a shift only 61.3% of patients had bilateral occlusion, one might want to look at the two hysteroscopic methods separately. Thirty-one women (32.6%) revealed a negative CDS fluid shift and were included in a sub-analysis. Using the air bubble technique, in all 11 patients, uni- or bilateral patency was predicted correctly (positive predictive value [PPV]: 100%, 95% CI: 64.8-100) and 19/20 patients with a bilateral negative air “bubble sign” had bilateral occlusion laparoscopic chromopertubation (negative predictive value [NPV]: 95.0%, 95% CI: 96.6-100; p<0.001).
Discussion
This secondary analysis of our previously published prospective study [8] suggests once again that hysteroscopic evaluation of tubal patency is feasible and reveals high overall accuracy. However, although a combination of the “bubble sign” and transvaginal sonography for the detection of changes in CDS fluid volume had previously been proposed by Parry et al. [5], however, it had remained open whether this combination would really increase the overall accuracy when compared to the single methods alone.
Notably, our data demonstrate that when both tools were applied simultaneously, uni-/bilateral patency could be predicted with a lower sensitivity (80.3%) than with the hysteroscopic “bubble sign” (94.7%) or peri-hysteroscopic sonography (83.3%) alone. Both the combined approach and the measurement of changes in CDS fluid volume led to a specificity of 100%. Thus, in terms of sensitivity and specificity, the combined approach does appear to be superior in distinguishing between unilateral/bilateral patency and bilateral obstruction, especially when compared to peri-hysteroscopic sonography alone. However, both the patient and the physician might be more interested in the individual chance of the examined patient, which is better reflected by the PPV and the NPV. The “bubble sign” led to a PPV of 94.7% for uni-/bilateral patency, which was exceeded by the two other methods (100%). Of note, the combined method revealed the lowest specificity (55.7%), which is likely due to the inaccurate performance of the peri-hysteroscopic sonography (NPV: 61.3%). In other words, only 19/31 women (61.3%) without any measurable CDS fluid shift finally revealed bilateral tubal occlusion in laparoscopic chromopertubation. Although the presence of a fluid shift is reassuring for the patient by means that at least one Fallopian tube is patent, one cannot rely on the result of peri-hysteroscopic sonography when bilateral tubal occlusion is suspected. Regarding this aspect, the “bubble sign” performed better. In detail, when both tubes revealed a negative “bubble sign”, the patients’ chance for bilateral occlusion was 78.9%.
Thus, depending on what one wants to prove, each method obviously has its advantages and disadvantages. It therefore seems reasonable to combine both methods, particularly since both are easy and quick to perform. Moreover, observing the “bubble sign” in addition to changes in CDS volume allows the physician to assess each Fallopian tube in an independent manner and to also suspect unilateral occlusion, which has been previously reported [5,6].
Accordingly, we would recommend the following strategy: in case of a positive fluid shift (increase in CDS volume after the hysteroscopy), the patient can be re-assured that at least one Fallopian tube is open with a probability bordering on certainty (PPV: 100%, Table 2). However, a statement about each individual tube is only possible with the air bubble technique as reported previously [5,6]. In case of a negative fluid shift, the situation is less clear, since only about 60% of women finally had bilateral occlusion. As demonstrated in our sub-analysis, in these patients, the air “bubble sign” allows good separation between those without and those with bilateral occlusion with high accuracy of about 100%. Thus, a sequential interpretation of the hysteroscopic results seems to bring the most reliable results.
Several study weaknesses need to be addressed: first, the examined patient population might not reflect a general infertile female population, since many women underwent laparoscopy for suspicion of endometriosis and tubal infertility per se, which obviously increased the rate of tubal damage. However, this allowed us to perform this analysis, since the incidence of bilateral tubal occlusion was comparably high (about 20%). Moreover, the exact pressure used for hysteroscopy could not be measured. The exact pressure needed to achieve patency in the course of chromopertubation could not be measured. Last but not least, the hysteroscopic procedures were performed under general anesthesia and, thus, the data might not be valid for outpatient hysteroscopy. However, there are also several strengths: the data were collected prospectively and the surgeons, who performed the hysteroscopic methods of tubal patency testing, were blinded to results of the laparoscopic chromopertubation and vice versa.
In conclusion, using the hysteroscopic “bubble sign” and peri-hysteroscopic sonography for the detection of changes in CDS volume are reliable methods to diagnose patency of at least one Fallopian tube. Moreover, especially the “bubble sign” is also potent in the prediction of bilateral occlusion. Performing both techniques when an infertile woman needs hysteroscopy is helpful in maximizing the informative output of the procedure.
Conflict of interests
The authors declare having no conflicts of interest.
Funding
None.