Introduction
Caesarean section (CS) delivery rates have risen dramatically worldwide over the last three decades [1]. In Canada, there has been a 50.8% increase between 1997 and 2016. In 2019, 288.80 per 1,000 live births (28.8%) were performed via caesarean delivery [1]. As surgical procedure rates increase and CS become one of the most common surgical procedures globally, the use of postpartum pain management has also risen [2]. Effective postpartum pain analgesia is essential for parent-child bonding and enhanced functional recovery as well as in the prevention of chronic pain and postpartum depression [2]. Novel regimens for pain management should focus on a balance between efficacy and safety.
Multiple modalities of postoperative analgesia are currently used in the immediate post-caesarean period, including NSAIDs and transversus abdominal plane (TAP) blocks [3]. However, the administration of opioids remains the gold standard and is the most frequently prescribed analgesic [3]. This presents many challenges due to the potentially dangerous and detrimental side effects and complications of this drug class [4]. In addition, the increase of prescribed opioid medications over the last few decades has been directly linked to a dramatic surge in opioid-related morbidity and mortality due to prescription diversion and addiction [5].
In 2017, approximately 68% of fatal drug overdoses in The United States were associated with opioids, driven by misuse of excess prescriptions and leftover tablets, leading to chronic opioid consumption and heroin abuse5. That same year, the U.S. Department of Health and Human Services declared the opioid epidemic a public health emergency in part due to the diversion and misuse of opioids prescribed for the treatment of acute pain, often following surgery [6]. While this had an impact, the opioid crisis continues. In 2020, 75% of 91,799 drug overdoses involved an opioid in The United States7. Similar concerns were raised in Canada. In 2018, roughly 3.7 million people over the age of 15 reported use of opioids for analgesic purposes. Of those individuals, roughly 351,000 engaged in problematic use [8]. According to the Government of Canada, Health Infobase, a total of 40,642 apparent opioid toxicity deaths between January 2016 and June 2023 [9].
The United States and Canada are the first and second-largest per capita consumers of opioids worldwide [10]. As such, due to the current opioid crisis, physicians have been called upon to reduce opioid prescribing and work towards finding alternative modes of postoperative analgesia [10]. In response to this epidemic, the Choosing Wisely Canada campaign – a national strategy to reduce unnecessary tests and treatments – has launched an Opioid Wisely campaign to encourage thoughtful opioid prescribing and minimize opioid-related harm.
In supporting the efforts of this campaign, this systematic review will focus on highlighting the recent quality improvement (QI) studies that concentrate on decreasing the use of opioids post-caesarean section delivery. Through this study, we hope to encourage the uptake and implementation of some of the effective methods employed to minimize unnecessary opioid prescriptions. Recent studies have shown that the use of QI initiatives post-caesarean section, such as enhanced recovery pathway after surgery (ERAS) and individualized patient analgesia plans substantially decrease opioid prescriptions, ranging from a 35% decrease in one study [11] to 97.9% in another [12]. Exploring the successful interventions implemented and their results is another step in combatting the opioid crisis and optimizing post-caesarean patient care.
Methods
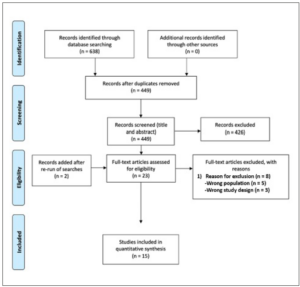
This literature review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement. The review protocol was registered in the PROSPERO database, registration number: CRD42022331519. The following databases were searched from inception to 14 April 2022 using a comprehensive search strategy which included the following databases: Ovid MEDLINE, PubMed (non-MEDLINE records only), Ovid Embase, Web of Science, Cochrane Central Register of Control Trials, and Cochrane Database of Systematic Reviews. Searches were conducted using relevant Medical Subject Heading (MeSH) terms and keywords related to opioids, narcotics, QI studies, and caesarean sections. Search results were managed using Endnote and screened using Covidence. The search was re-run prior to submission on 10/20/2022, and two new studies were identified and included. Selected studies included quality improvement studies only.
Initially, 638 studies were retrieved. After duplicate were removed, a total of 449 studies were identified based on our search strategy. Titles and abstracts were screened through Covidence and a further 326 studies were dismissed leaving 23 full text studies for review. After additional exclusion based on eligibility of studies, 15 studies met the inclusion criteria and were included for further full text review (Figure 1). A total of 13,319 patients have been included in QI studies aimed at decreasing the use of opioids post-caesarean delivery. Data was recorded in a table with the following factors extracted: Author, Country, Intervention used, Number of patients, and Results (Table 1).
Results
All studies were undertaken at academic, tertiary, urban or suburban medical centers in the United States (93.3%) or Canada (6.7%). Pre- to post- study designs were utilized, such that outcomes were before and after the QI initiative was implemented, with a “washout” period in between during which no data was collected. Pre-intervention and post-intervention data were collected using Electronic Medical Record (EMR) and/or surveys for women who underwent caesarean delivery at the setting [11-25].
While the interventions varied in type and duration, common approaches include enhancing patient and staff education, increasing the use of non-opioid analgesics, emphasizing shared decision-making, and implementing a maximum quantity of opioids prescribed at time of discharge. Trends in findings were similar across all studies; this included reduction in opioid prescription both in-patient and at discharge and increased use of non-opioid pain control measures, particularly acetaminophen. All studies demonstrated an improvement or no significant changes to pain scores and/or patient satisfaction with pain control [11-25].
The most common intervention used was ERAS, which was employed by 4 out of 15 studies [13-16]. This included but was not limited to multimodal pain control with pharmacologic and non-pharmacologic interventions, dietary modifications, early postoperative return to oral intake and ambulation, and improved pre- and postoperative education on pain control and recovery expectations [13-16]. Notably, Hedderson et al. also decoupled opioids from other medications to facilitate maximization of acetaminophen use before addition of opioids16. Findings were similar across studies and showed a significant decrease in morphine milligram equivalents (MME) consumption in an in-patient setting [13-16], an increase in the use of non-opioid analgesics [16], improvement [13,16] or no significant difference in reported pain score [14] and decreased [14] or no significant change [15,16] in the length of hospital stay. In addition, Hedderson et al. demonstrated decreased time to first post-surgical ambulation [16], and Tepper et al. demonstrated decreased prescription of opioids at discharge [15].
Three studies used the Plan, Do, Study, Act (PDSA) or Plan, Do, Check, Act (PDCA) model for QI [11,12,17]. Specifically, Kahn et al. developed a standardized visual tool to facilitate integration of women’s preferences in their post-caesarean delivery care and emphasize routine use of non-pharmacological pain management measures. There was an observed 79% reduction in the total in-patient opioid consumption, with 85% of patients reporting their pain to be controlled at a satisfactory level [17]. Similarly, Prabhu et al. employed a two-phase QI protocol that implemented 1) discharge counselling with shared decision-making on the quantity of opioids to be prescribed, up to a maximum of 30 tablets of 5 mg oxycodone, and 2) standardized prescribing of ibuprofen and acetaminophen in both in-patient and out-patient settings. Opioid prescriptions post-discharge decreased by 35% (p<0.01), from a mean of 33.2 to 21.5 tablets (p<0.01). While ibuprofen was prescribed at high rates throughout the study, acetaminophen prescription rates increased from 32.6% to 92.0% (p<0.001) [11]. Lastly, Lakhi et al. implemented a restrictive prescribing policy, whereby physicians were not allowed to prescribe opioids upon discharge after caesarean delivery, but patients may call to request additional analgesia if necessary. As a result, opioid prescriptions at discharge decreased from 97.9% to 0%. 18% of women requested opioid prescriptions post-discharge, and only 51% filled the prescription. Pain control was reported as satisfactory in 89.7% of patients. Notably, patient factors associated with opioid consumption included white race, multiparity, and opioid consumption during their inpatient stay [12].
Three studies investigated the efficacy of single-method interventions in reducing opioid use post-caesarean delivery [18,19,25]. Similar to Prabhu et al., Loomis et al. developed a shared decision-making tool focused on patient education, multimodal pain control, and safe storage and disposal of excess medications. Women were allowed to choose up to 30 tablets of 5 mg oxycodone and were given a home opioid deactivation system to dispose of excess tablets. On average, participants selected 18 tablets and consumed 13 tablets. Interestingly, 37% of participants felt that they received just enough medication to adequately control pain, while 55% of participants felt that they received too much [18]. Next, Kim et al. used the DMAIC (design, measure, analyze, improve, control) protocol to develop a post-caesarean section opioid prescription algorithm based on chart review and validated surveys. Post-intervention, mean prescription at discharge decreased from 17.6 MMEs to 8.4 MMEs (p<0.01), with a 23% increase in women discharged without a prescription (p<0.01). There were no differences in patient satisfaction or pain perception [19]. Finally, Voelker et al. used an academic detailing intervention that provided baseline data and remeasurement to all delivering providers, including obstetricians, family physicians, and nurse-midwives. Opioid prescription rates decreased from 100% to 93% in post-caesarean deliveries (p=0.054), alongside a decrease in number of tablets (p=0.0002) [25].
Five studies utilized other combinations of interventions to reduce opioid use post-caesarean delivery [20-24]. Burgess et al. designed a comfort bundle that consisted of standardized use of pre-operative acetaminophen, postoperative comfort education, simethicone, postoperative gum chewing, and abdominal binders. MME use in-patient was reduced by 61% and the proportion of women prescribed <20 tablets of 5 mg oxycodone increased from 26.3% to 96.7%. Patient satisfaction scores on pain control showed improvements post-intervention [20]. Laksono et al. employed a bundled QI intervention consisting of opioid prescribing instructions in resident physician orientation, nursing and patient education, and standard electronic prescriptions consisting of 10 tablets of 5 mg morphine or 5 tablets of 1 mg hydromorphone if requiring opioids. The quantity of opioids prescribed at discharge decreased from 97.6 MMEs to 35.8 MME (p<0.001), with no post-intervention visits to the clinic due to insufficient pain control [21]. Next, Holland et al. eliminated routine use of opioids post-caesarean delivery by implementing a short course of opioids when necessary, utilizing in-patient opioid use patterns to determine prescription at discharge, and shared decision-making. There was a 23% reduction in in-patient opioid use (p<0.001), from a median of 60.0 MME to 52.5 MME (p=0.05). The proportion of women prescribed opioids at discharge decreased from 91% to 40% (p<0.001). Among those who were prescribed opioids, the median quantity decreased from 157.5 MME to 112.5 MME (p<0.001). There were no changes to pain scores or patient satisfaction in pain control [22].
Like Hedderson et al., 2 other studies also incorporated decoupling opioids from other medications [23,24]. Llarena et al. designed Reduced Option for Opioid Therapy (ROOT), which maximized the use of NSAIDs and acetaminophen, physician and nursing education, and data-driven nursing feedback. Median in-patient opioid use decreased by over 60% from 75 MME to 30 MME (p<0.001), while median opioid prescription at discharge decreased from 210 MME to 150 MME (p<0.001). There was a decrease in pain scores post-intervention (p<0.001) [23]. Smith et al. employed a similar in-patient approach involving decoupling of opioids from acetaminophen, scheduled administration of NSAIDs and acetaminophen, and limitation of opioid use to breakthrough pain. There was a 75% reduction in median in-patient opioid use, from 120 MME to 30 ME (p<0.001). While ketorolac and ibuprofen use did not change, there was an increase in acetaminophen use (p<0.001). There was no difference in pain scores or length of hospital stay [24].
Discussion
The use of opioids remains the gold standard for post-caesarean section analgesia, but they have many detrimental side effects such as sedation, constipation, respiratory depression, tolerance, and physical dependence, and the potential for fatal toxicity [4,26]. In the United States and Canada, the majority of drug-related morbidity and mortality is related to opioid misuse [7-9]. This is exacerbated by excess prescriptions and the diversion of leftover tablets given for acute pain management and following surgery [5]. Several studies have assessed various strategies to minimize the adverse events related to opioids including symptomatic management, dose reduction, opioid rotation, and altering route of administration [27,28]. However, the majority of these studies were focused on chronic pain management in an older population and were not specified to post-caesarean care.
To minimize the administration of opioids in the post-caesarean period, the efficacy of alternative interventions has been evaluated through numerous studies. These include enhancing patient and provider education, highlighting shared decision-making and increasing the frequency or duration of non-opioid analgesia. The most studied non-opioid techniques include TAP block, NSAIDs and IV paracetamol [3]. Other analgesics, such as ketamine, ilioinguinal-iliohypogastric nerve block, and wound infiltration with local anesthetic may be used in specific cases, however their efficacy has been less studied [3]. Further research is still needed to guide physician decision-making on optimal pain control options to increase the use of non-opiate modalities for long-term safety while maintaining or improving overall patient satisfaction.
In this systematic review, 4 out of 15 studies (25%) implemented ERAS [13-16]. ERAS is a multidisciplinary program that aims to optimize patient recovery post-operatively while reducing opiate exposure, and consequently the incidence of substance use disorder. ERAS encourages early return to function, reducing the length of hospital stay, and decreasing the rate of post-surgical complications [16,29]. The utilization of ERAS programs in patients undergoing caesarean section resulted in a reduction of inpatient and outpatient opioid exposure without worsening surgical outcomes [15,16]. Where opioids were used for pain control, the dose or the average number of pills prescribed was decreased [13,16]. Although this has been the most studied QI initiative, it is unclear if ERAS alone was the most effective as studies utilizing alternate approaches have demonstrated greater results in reduction of opioid use.
Our results show that there are a multitude of initiatives that can be implemented to reach the same goal: a reduction in opioid use post-caesarean delivery. In addition to ERAS, other interventions studied included a combination of discharge counselling and patient education, shared decision-making on the quantity of opioids to be prescribed, restrictive prescribing policies to maximize NSAIDs and acetaminophen use, and comfort bundles consisting of non-opioid analgesia, simethicone, postoperative gum chewing, and abdominal binders [11,12,18,20]. Overall, the implementation of these interventions reduced inpatient opioid consumption and decreased post-discharge opioid prescriptions with improved patient satisfaction on pain control.
Of the studies included in this paper, 100% of them were performed in North America [11-25]. To further expand on this topic, additional research needs to be implemented by clinicians worldwide to tackle the ongoing opioid crisis and share strategies on minimizing postpartum pain. Educating patients on alternative pain control methods, involving them in decisions regarding their postoperative pain management, and maximizing the use of non-opioid medications can reduce overall opioid consumption and shorten the length of hospital stay without influencing their perception of pain relief or increasing complications and readmission rates. Providing patients with methods to safely dispose excess tablets can also reduce the number of tablets available for misuse or diversion into the community. Implementing a combination of these strategies can potentially prevent opioid-naïve patients from experiencing adverse side effects from opioids post-caesarean delivery and decrease the number of opioids that may be potentially diverted and misused in our communities.
Conclusion
There is a multitude of convincing and impactful data to demonstrate that reducing the use of opioids after caesarean delivery via alternative safer approaches is possible and highly achievable. Each study included in this systematic review showed a statistically significant decrease in opioid use and prescription once a QI initiative was implemented thus decreasing the opioid related risk to both postpartum patients and the wider community. While it is known that the United States and Canada are the largest per-capita consumers of opioids worldwide [10], further work on quality improvement strategies should be performed in other settings to further enhance the reliability and acceptability of effective interventions worldwide. Despite the risks associated with them, opioids continue to be the gold standard for postoperative pain control. Thus, further research is needed to explore alternative non-opioid, yet equally effective analgesic options post-caesarean section to shift the focus to safer alternatives. By highlighting effective QI strategies, this systematic review aims to push forward the efforts of the Opioid Wisely Campaign in Canada and encourage physicians managing post-caesarean pain to choose wisely when determining treatment modalities for the good of both the postoperative patient and the overall health of our communities.
Conflicts of interest
The authors declare having no conflicts of interest.